
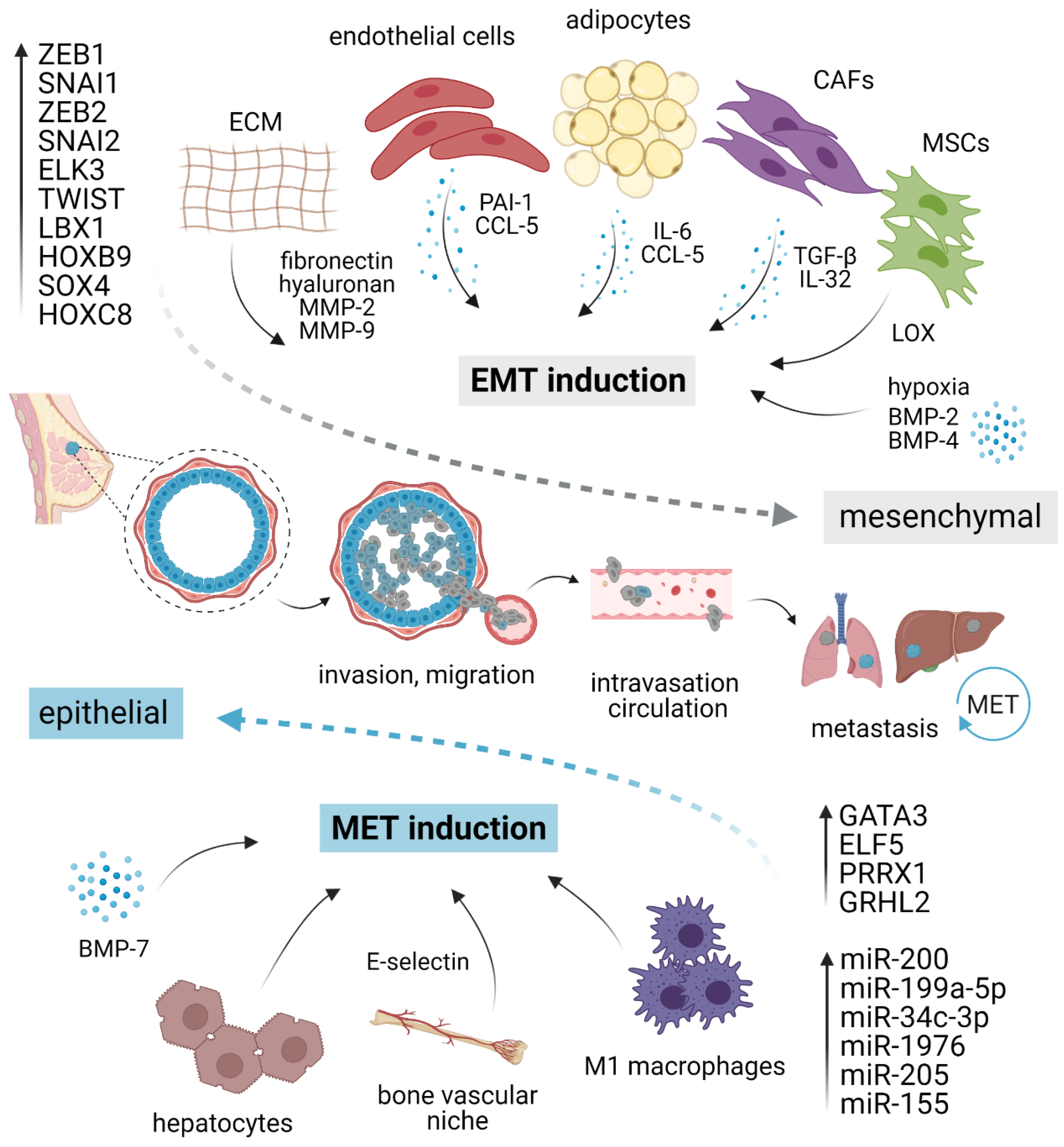
But once again, many chemotherapies, none of them very appealing. In this case, probably the fact that the patient received it in the post-neoadjuvant setting makes it less appealing. It’s usually an active agent that’s oral, and doesn’t have much alopecia. I agree that capecitabine is a great agent. For a case that was not showing AST and ALN elevations, maybe then a visceral disease. But for the time being, chemotherapy remains the mainstay here. And, once again, we hope that this can turn tumors into more immunogenic and can lead to a benefit with immunotherapy. We are running the Saci-IO trials that is combining sacituzumab with or without the addition of pembrolizumab in this setting. But we’re looking at trials that try to combine immunotherapy, even in this subset of patients, to see if we can somehow turn cold tumors into hot tumors.Īnd, once again, thinking about conjugates that are a class of drugs that we believe could help in this sense. And it’s unfortunate, of course, that we cannot use immunotherapy because of the PD-L1 CPS. That is not ideal but, in this setting, it can really help the patient.
Triple negative breast cancer prognosis trial#
We’ve seen in the TNT trial that they both can achieve around a 30% response rate. And the thing is that, of course, in this case, the patient has already received toxins and never received platinum, and this might make me think of platinum. I feel that in the first line, of course, for such an aggressive disease, like triple-negative breast cancer that has relapsed and has visceral disease, I would think of infusive chemotherapy for something like taxanes or carboplatin. Paolo Tarantino, MD: Well, I totally agree with you. Or in a patient who, for example, had a different site, not liver, but a different site of cancer, I might think about capecitabine. A lot of people use gemcitabine and carboplatin, but I have to say that in a patient like this, I tend to give first-line chemotherapy with either a taxane, where I think we have some inferential data suggesting it might be a little bit better, and I give nab-paclitaxel. There’s a lot of discussion about what chemotherapy to use. She’s quite far out, more than a year, which usually is our differentiation in terms of trying to decide what to do and our standard in the first-line setting is chemotherapy. So that means that she goes out of that arm of our stepwise process and uses a checkpoint inhibitor and we’re really left with chemotherapy in the first-line setting.
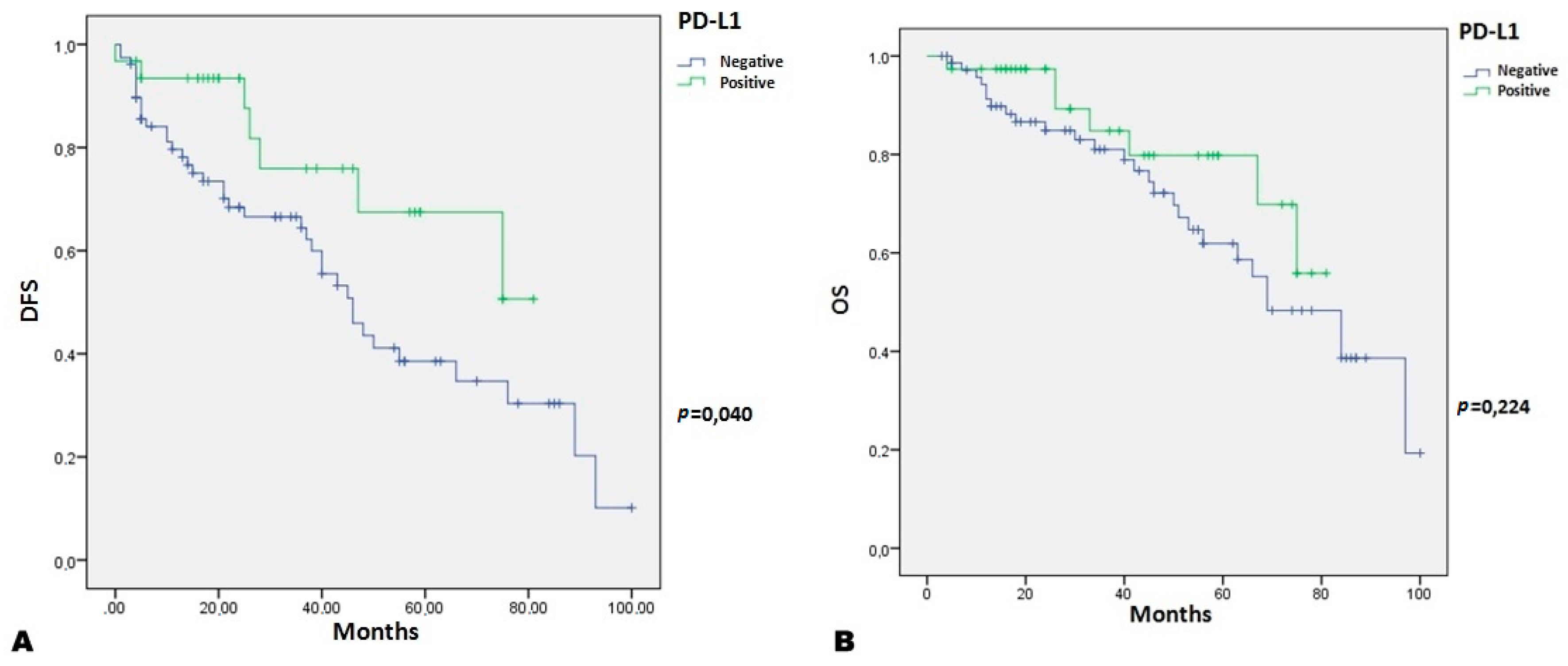
She has PD-L1 testing, and with the combined positive score, it’s less than 10%. And I will say that one of the questions that come up is what tumor sample you use to determine HER2-low? And we’ll talk about that in just a moment.īut the first thing that we do when we’re looking at a patient like this, other than feel really sorry that they have recurrent disease, is to first look to see whether or not they’re eligible for pembrolizumab from the KEYNOTE-355 trial, which showed improved survival with the addition of pembrolizumab in that setting. She has imaging that shows multiple liver lesions and a biopsy, which is critical, I think, in this setting, that shows that she has triple-negative breast cancer.

A good performance status but still symptomatic. Has a 1 ½ time elevation of her liver enzymes.
She finished all her treatment in September 2020 and she didn’t have recurrent disease again until June 2022, when she comes in with symptoms that are really consistent with having liver metastases, fatigue, and right upper quadrant discomfort. Rugo, MD, FASCO: This patient has a longer time to recurrent disease.


 0 kommentar(er)
0 kommentar(er)
